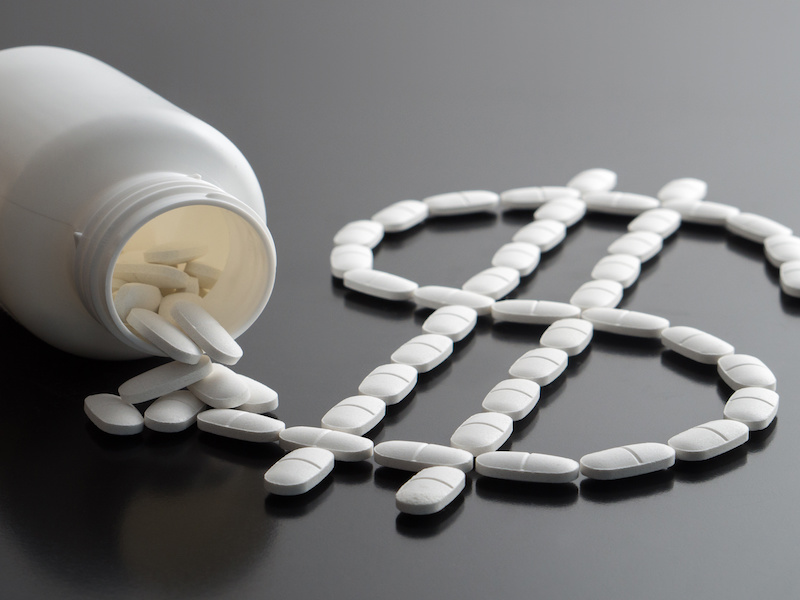
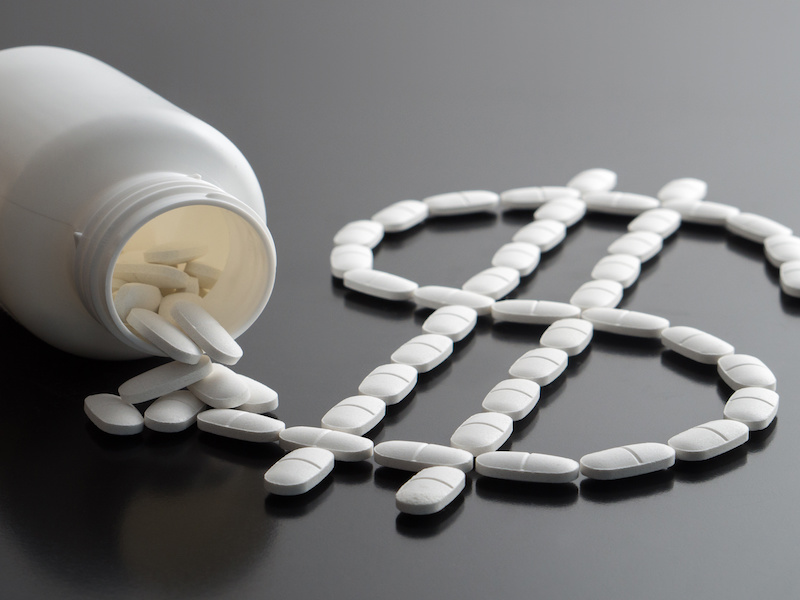
Canadian plan sponsors and insurers are revisiting how they classify obesity drugs under their benefits plans, amid plan members’ rising demand for Ozempic as a weight-loss treatment.
Ozempic, also known under the generic name semaglutide, is a drug used to treat type 2 diabetes. However, the medication has also been credited as a weight-loss treatment, which people struggling with obesity have called a game-changer.
According to a recent report by Express Scripts Canada, semaglutide was the top traditional drug by overall spend for private drug plans in both 2021 and 2022. It also generated the highest drug spend per claimant in 2022 and was the primary cost driver for the diabetes therapeutic class for that category of drugs. The annual drug spend per claimant was also significantly higher for semaglutide (roughly $1,500) compared to other diabetes treatments such as metformin (around $100). The report also found semaglutide was the drug treatment for fewer than a third (31 per cent) of patients with type 2 diabetes.
Read: Annual spend per private drug plan member up 6.3% in 2022: report
Based on Express Scripts Canada’s report, the number of claimants for semaglutide doesn’t align with the number of patients with type 2 diabetes, says Suzanne Lepage, a private health plan strategist. “It suggests that Ozempic is being prescribed by doctors off label as a weight-loss drug.”
Until now, Ozempic wasn’t subject to prior authorization, so insurers were unaware of the conditions for which it was being prescribed, she says, noting since physicians aren’t prohibited from prescribing drugs off label, they can use their discretion in determining the right treatments for patients.
Several insurers have taken steps to ensure Ozempic is used for its indication. Medavie Blue Cross uses tiered copay plans and step therapy plans to ensure first-line diabetes treatments have preferential coverage over Ozempic and similar second-line drugs, according to a post on the insurer’s website. Beneva Inc. is also implementing cost containment measures, such as prior authorization and automated step therapy, to ensure optimal drug cost control.
Novo Nordisk, which manufactures Ozempic, has since developed a semaglutide drug formulation marketed under the brand name Wegovy, specifically indicated for weight loss. While Wegovy was approved by Health Canada in 2021, it still isn’t commercially available in Canada, leading physicians to continue prescribing Ozempic for their patients living with obesity and at increased costs to private plans.
Since private drug plans have historically classified obesity as a ‘lifestyle choice,’ most plans typically don’t cover drugs for this condition. Experts have long advocated for employers to treat obesity as a chronic condition in order for these treatments to be covered under their benefits plans.
Read: Specialty drug prior authorization a useful tool for plan sponsors
“Many employers are reconsidering their position on covering anti-obesity drugs because they understand it’s a medical condition that has co-morbidities, so helping people on that [health] journey helps mitigate risk associated with other medical conditions as well,” says Kim Siddall, national vice-president of account management of mid- and large-sized markets at People Corporation Inc.
While many insurers, such as Medavie Blue Cross and Equitable Life Insurance Co. of Canada, have indicated they won’t cover semaglutide as an off-label prescription, the jury is out on whether they’ll cover Wegovy. Indeed, in its website post, Medavie said upwards of 50 per cent of its block of groups now provide access to weight-loss medications for their members and weight-loss drugs are now standard coverage through its formulary, but these drugs require prior authorization to validate they’re being used to treat obesity. The insurer said plan sponsors that prefer not to apply prior authorization can manage this category of drugs with an annual plan maximum.
The changing view on the causes of obesity is now medically driven, says Siddall, noting it’s part of a broader push by plan sponsors and insurers towards diversity, equity and inclusion benefits. “It’s helping people get the treatment supports they need to live their best lives and be healthy at work. But it also is another way employers can show employees support and allow them to bring their authentic selves to work.”
Read: Update benefits plans, workplace policies to treat obesity like any chronic disease
